Neurons of the reticular formation. Dysfunction of the reticular formation. The nuclei of the reticular formation and their functions
The variety of functions performed by different parts of the reticular formation is presented in the table below.
a) Motion program generators... Cranial nerve movement programs include the following:
Concomitant (parallel) eye movements, locally controlled by motor nodes (gaze centers) in the midbrain and pons, which have a connection with the nuclei of the motor nerves of the eyes.
Rhythmic chewing movements controlled by the supratrieminal premotor nucleus of the pons.
Swallowing, gagging, coughing, yawning and sneezing control the individual premotor nuclei of the medulla oblongata, which are connected with the corresponding cranial nerves and the respiratory center.
The salivary nuclei are referred to as the small-cell reticular formation of the pons and the medulla oblongata. Preganglionic parasympathetic fibers depart from them to the facial and glossopharyngeal nerves.
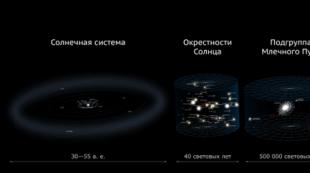
Reticular formation(RF).(A) Departments. (B) Groups of aminergic and cholinergic cells.

1. Motion program generators... From experiments on animals it has long been established that the generators of the movement programs of lower vertebrates and lower mammals are located in the gray matter of the spinal cord, connecting with the help of nerves to each of the four limbs. These generators in the spinal cord are electrical neural networks that sequentially deliver signals to flexor and extensor muscle groups. The generative activity of the spinal cord obeys commands from the higher centers, the motor region of the midbrain (DOSM).
DOSM includes the leg-bridge nucleus, adjacent to the superior cerebellar peduncle in the place of its passage in the region of the upper edge of the fourth ventricle and junction with the midbrain. Descending fibers depart from these nuclei as part of the central tegmental pathway to the oral and caudal nuclei of the pons, formed by motor neurons that innervate the extensor muscles, and to the large cell neurons of the medulla oblongata, which control neurons that innervate the flexor muscles.
The main mechanism of rehabilitation for spinal cord injuries is the activation of spinal motor reflexes in patients who have suffered injuries with partial or complete rupture of the spinal cord. It is now well known that even after a complete rupture at the level of the cervical or thoracic spine, it is possible to activate the lumbosacral movement programs by continuous electrical stimulation of the dura mater at the level of the lumbar segments. Stimulation largely activates the dorsal root fibers, triggering impulses at the base of the anterior horn.
Surface electromyography (EMG) from flexor and extensor muscles showed consistent excitation of neurons in flexor and extensor muscles, although this program did not correspond to normal. For the formation of a normal program, the rupture must be incomplete with the preservation of a part of the descending paths from the leg-bridge nucleus.
The creation of true stepping movements with a complete rupture is possible if the patient is placed on a treadmill with simultaneous stimulation of the dura mater, mainly due to the generator receiving additional sensitive and proprioceptive impulses. Muscle strength and walking speed will build up over several weeks, but not enough to walk without using a walker.
Modern research is aimed at improving the ability to "create a bridge" with supraspinal motor fibers by clearing tissue debris at the site of rupture and replacing these tissues with a composition that physically and chemically stimulates axonal regeneration.
2. Higher Centers for Urinary Control are described in the following article on the site.
 General scheme of movement control.
General scheme of movement control.
b) Breathing control... The respiratory cycle is largely regulated by the dorsal and ventral respiratory nuclei, located in the upper part of the medulla oblongata on each side of the midline. The dorsal respiratory nucleus is located in the mid-lateral nucleus of the solitary tract. The ventral nucleus is located behind the double nucleus (hence the name - the posterior double nucleus). It is responsible for exhaling; since this process normally occurs passively, the activity of neurons during normal respiration is relatively low, but it increases significantly under exertion. The third, medial parabrachial nucleus, adjacent to the macula macula, is likely to play a role in the breathing mechanism that occurs in the waking state.
Parabrachial nucleus, formed by many subgroups of neurons, together with the above-described aminergic and cholinergic systems, is involved in maintaining a state of wakefulness by activating the cerebral cortex. Stimulation of this nucleus by the amygdala in anxiety disorders results in characteristic hyperventilation.
Dorsal respiratory nucleus controls the inhalation process. From it, fibers extend to motor neurons on the opposite side of the spinal cord, which innervate the diaphragm, intercostal and auxiliary respiratory muscles. The nucleus receives ascending excitatory impulses from the chemoreceptors of the chemosensitive region of the medulla oblongata and the carotid sinus.
Ventral respiratory nucleus responsible for exhalation. When breathing calmly, it works as a neural circuit, participating in reciprocal inhibition of the inspiratory center by means of GABAergic (γ-aminobutyric acid) intercalary neurons. With forced breathing, it activates the cells of the anterior horn, which innervate the abdominal muscles, which are responsible for the collapse of the lungs.
1. Chemosensitive region of the medulla oblongata... The choroid plexus of the fourth ventricle produces cerebrospinal fluid (CSF) passing through the lateral aperture (Lushka) of the fourth ventricle. The cells of the lateral reticular formation on the surface of the medulla oblongata in this area are extremely sensitive to the concentration of hydrogen ions (H +) in the washing CSF. In fact, this chemosensitive region of the medulla oblongata analyzes the partial pressure of carbon dioxide (pCO 2) in the CSF, which corresponds to the pCO 2 of the blood supplying the brain. Any increase in the concentration of H + ions leads to stimulation of the dorsal respiratory nucleus by direct synaptic communication (several other chemosensitive nuclei are located in the medulla oblongata).
2. Carotid sinus chemoreceptors... The carotid sinus, the size of a pinhead, is adjacent to the trunk of the internal carotid artery and receives a branch from this artery that branches out inside. The blood flow through the carotid sinus is so intense that the arteriovenous oxygen partial pressure (pO 2) changes by less than 1%. Chemoreceptors are glomerular cells innervated by branches of the sinus nerve (branch IX of the cranial nerve). Carotid chemoreceptors respond to both a decrease in pO 2 and an increase in pCO 2 and provide reflex regulation of blood gas levels by changing the respiratory rate.
The chemoreceptors of the aortic glomus (under the aortic arch) in humans are relatively underdeveloped.
 Respiratory center. All slices are shown from below and from the back.
Respiratory center. All slices are shown from below and from the back. (A) - enlarged cut (B).
(A) Inhibitory interaction between the dorsal and ventral respiratory nuclei (DSP, VDN).
To the chemosensitive area (CCR) of the medulla oblongata, the fibers from which are directed to the DNF, there are capillaries of the choroid that produce cerebrospinal fluid (CSF) (B).
As part of the glossopharyngeal nerve (IX), chemosensitive fibers pass from the carotid sinus to the DNF.
(C) Excitation of the motor neurons of the diaphragm carries out the opposite DFN.
(D) For forced expiration, the VDJ of the opposite side excites the neurons of the muscles of the anterior abdominal wall.
v) Control of the cardiovascular system... Cardiac output and peripheral vascular resistance regulate the nervous and endocrine systems. Due to the wide spread of essential arterial hypertension in late middle age, most studies in this area are aimed at studying the mechanisms of cardiovascular regulation.
The ascending fibers that signal high blood pressure start from stretch receptors (numerous free nerve endings) in the wall of the carotid sinus and the aortic arch. These ascending fibers, known as baroreceptors, travel to the medially located cells of the solitary tract nucleus that form the baroreceptor center. Ascending fibers from the carotid sinus pass through the glossopharyngeal nerve; fibers from the aortic arch are part of the vagus nerve. Baroreceptor nerves are referred to as "buffer nerves", since their action is to correct any deviations in blood pressure from the norm.
Cardiac output and peripheral vascular resistance depend on the activity of the sympathetic and parasympathetic nervous systems. Two main baroreceptor reflexes - parasympathetic and sympathetic - help to normalize high blood pressure.
 :
:
(A) Upper medulla oblongata.
(B) Segments of the spinal cord from T1 to L3.
(B) The posterior wall of the heart. Baroreceptor reflex (left):
1. Stretch receptors in the carotid sinus excite the fibers of the sinus branch of the glossopharyngeal nerve. ICA-internal carotid artery.
2. Baroreceptor neurons of the nucleus of the solitary pathway respond by firing the heart-inhibiting (cardio-inhibiting) neurons of the dorsal (motor) nucleus of the vagus nerve (DN-X).
3. Preganglionic parasympathetic cholinergic fibers of the vagus nerve form synapses with cells of intramural ganglia in the posterior wall of the heart.
4. Postgangionic parasympathetic cholinergic fibers inhibit the pacemaker activity of the sinoatrial node, thereby reducing the heart rate.
Barosympathetic reflex (right):
1 Afferent fibers of the stretch receptors of the carotid sinus excite the medial baroreceptor neurons of the nucleus of the solitary pathway.
2. Baroreceptor neurons respond by firing inhibitory neurons of the depressor center in the central reticular nucleus of the medulla oblongata.
3. Inhibition of adrenergic and noradrenergic neurons of the pressor center of the lateral reticular nucleus (anterior ventrolateral part of the medulla oblongata) occurs.
4. Reduced tonic excitation of neurons in the lateral horns of the spinal cord.
5 and 6. Pre- and postganglionic inhibition of sympathetic innervation of arteriole tone occurs, which, in turn, leads to a decrease in peripheral vascular resistance.
G) Sleep and wakefulness... With electroencephalography (EEG), characteristic patterns of the electrical activity of cortical neurons can be observed in different states of consciousness. The normal state of wakefulness is characterized by high-frequency, low-amplitude waves. Falling asleep is accompanied by low-frequency high-amplitude waves, a higher wave amplitude is due to the synchronized activity of a larger number of neurons. This type of sleep is called slow-wave (synchronized) sleep or He-REM sleep (REM-rapid eye movement). It lasts about 60 minutes, and then goes into desynchronized sleep, in which the sequences on the EEG resemble those in the waking state. Only during this period do dreams and rapid eye movements occur (hence the more commonly used term - REM sleep). During a normal night's sleep, several cycles of REM sleep and non-REM sleep follow each other, described in a separate article on the website.
The alternation of sleep and wakefulness cycles is a reflection of two neural networks in the brain, one operating in a waking state and the other in a sleep state. These networks are opposed to each other as a "switch" between sleep and wakefulness (which makes it possible to switch between networks quickly and completely). A similar pattern works when changing from REM sleep to slow-wave sleep. Normally, sleep is controlled by physiological systems (the contribution of the homeostasis system is a change in the level of cell metabolism), circadian rhythms (the suprachiasmal nucleus is the main biological clock that is synchronized with information from the environment, the effect of light on the retina and melatonin produced by the pineal gland, and control sleep-wake cycle and other physiological functions) and allostatic load (food intake and physical activity).
These factors change slowly, and without a rapid change in the state of the switching mechanism, the transition from wakefulness to sleep would also be slow and uncomfortable.
3. Stimulation of awakening, or activating systems(caudal midbrain and rostral pons). For the activation of the cortex large hemispheres there are two main ways:
Cholinergic neurons (of the pons and laterodorsal tegmental nuclei) approach the thalamus (switching nuclei and reticular nucleus) and inhibit those GABAergic neurons of the thalamus, whose task is to prevent the transmission of sensitive information to the cerebral cortex.
Monoaminergic neurons are located in the macula macula, the dorsal and median nuclei of the suture (serotonergic), the parabrachial nucleus (glutamatergic), the periaqueductal gray matter (OVSV, dopaminergic) and in the serotus-mastoid nucleus (histaminergic). The axons of the neurons in each of these areas are directed to the basal regions of the forebrain (the basal nucleus of Meinert and the unnamed substance), and from there to the cerebral cortex.
Peptidergic (orexin) and glutamatergic neurons of the lateral hypothalamus, as well as cholinergic and GABAergic neurons of the basal forebrain ganglia also send fibers to the cerebral cortex.
Summary: biological basis attention is an orienting reflex.
I.P. Pavlov described the orienting reflex as an unconditioned reflex serving as the basis involuntary attention... The very same processes of attention in his system are explained, first of all, due to the interaction of excitation and inhibition, occurring in the cerebral cortex. When a person is attentive to something, it means that a focus of excitation arises in his cerebral cortex. At the same time, all other parts of the brain are in a state of inhibition. Therefore, a person who is focused on one thing may not notice anything else at that moment. But these ideas about brain relationships are too abstract. To be convinced of this, it is worth comparing this approach with the approach of A.R. Luria.
The teachings of A.R. Luria. In the teachings of A.R. Luria about the cerebral localization of higher mental functions of a person, a structural-functional model of the brain is given, in which each higher mental function is performed due to the joint work of three brain blocks (Luria A.R. Fundamentals of neuropsychology. M., 1973). The first block (block of regulation of the level of general and selective activation of the brain) is formed by nonspecific structures of the reticular formation of the brainstem, structures of the midbrain, diencephalic regions of the trunk, limbic system, mediobasal regions of the cortex of the frontal and temporal lobes of the brain. The second block (the block for receiving, processing and storing modal-specific information) is formed by the main analyzer systems (visual, auditory, skin-kinesthetic), the cortical zones of which are located in the posterior parts of the cerebral hemispheres. The third block (a block of programming, regulation and control over the course of mental function, providing the formation of motives for activity and control over the results of activity through a large number of bilateral connections with cortical and subcortical structures) is formed by the motor, premotor and prefrontal sections of the cerebral cortex. At the same time, the sequence of the work of these structures is important: at the first stage, an incentive to activity occurs, the basis of which is, among other things, the activation of the reticular formation.
The role of the reticular formation. The ability to be alert, reacting sometimes to a very slight change in environment, is provided by networks of nerve pathways located in the cerebral hemispheres that connect the reticular formation (a set of brain structures that regulate the level of excitability) with different parts of the cerebral cortex. Nerve impulses traveling along this network arise together with signals from the senses and excite the cortex, bringing it into a state of readiness to respond to further anticipated stimuli. Thus, the reticular formation with its ascending and descending fibers, together with the sense organs, causes the appearance of an orientation (or orientation-exploratory) reflex, being the primary physiological basis attention.
Back in 1935, F. Bremer compared electroencephalograms for two types of transection of the brain stem: a) at the level of the cervical vertebrae (a drug called "encephale isole" - the lower sections of the trunk) and b) at the level of the bridge (drug "cerveau isole" - upper sections of the trunk). In the first case, the records of bioelectrical activity did not differ from the EEG of normal animals, while in the second case, slow waves of large amplitude, characteristic of the state of sleep, were constantly present in the EEG. In preparations called "cerveau isole", only visual and olfactory afferent stimuli reach the cortex, since signals transmitted by other cranial nerves (in particular, auditory and trigeminal) are cut. Hence, F. Bremer concluded that when the central nervous system loses most of the stimulation coming from the outside world, sleep occurs; accordingly, maintaining a state of wakefulness is the result of an activating influence exerted by sensations. As D. Lindsley showed later, in these cases the signals caused by sensory stimuli continue to reach the cortex, but the electrical responses of the cortex to these signals become only short-lived and do not cause permanent changes. This showed that for the emergence of persistent processes of excitation that characterize the state of wakefulness, one influx of sensory impulses is not enough, a supporting effect of the activating reticular system is necessary.
These ideas about the processes of general activation received further development in the works of G. Moruzzi and G. Megun (Moruzzi G., Magoun H. W. Brain stem reticular formation and activation of the EEG // EEG and Clinical Neurophysiology. 1949, 1 - "Reticular formation of the brain stem and the activation reaction in the EEG"). They conducted experiments based on electrical stimulation of the brain, which revealed the functions of the nonspecific system of the brain - the reticular formation of the brainstem, which, along with the limbic system, belongs to the "modulating" systems of the brain. The main function of these systems is the regulation of the functional states of the body. The researchers did not turn off, but irritated the ascending reticular formation with electrodes implanted into it, showed that such stimulation of the reticular formation leads to the awakening of the animal, and further intensification of these irritations leads to the emergence of pronounced effective reactions of the animal. It turned out that when it is irritated with an electric current, an activation reaction occurs, and when this structure is removed, a coma occurs. These structures are actually responsible for maintaining a state of wakefulness, and the degree of their activity itself depends in part on sensory influences. However, contrary to what Bremer assumed, the activating influence of sensing does not manifest itself in the form of direct activation of the cerebral cortex by specific signals; it acts primarily on the reticular formation, the activity of which, in turn, regulates the functional state of the cortex, motor and vegetative centers. It was found that the cortical sleep of Bremer's "cerveau isole" preparations was caused not by the cutting of specific sensory pathways to the cortex, but by the elimination of the influences exerted on it by the reticular formation.
Also in the experiments of D. Lindsley it was revealed that stimulation of the stem nuclei of the ascending activating reticular formation significantly lowers the thresholds of sensitivity (in other words, sharpens the sensitivity) of the animal and allows for subtle differentiations (for example, differentiation of the image of a cone from the image of a triangle), which were previously inaccessible to the animal. ...
Neuroanatomy of the reticular formation. Initially, it was believed that the nonspecific system of the brain, which performs the task of diffuse and generalized activation of the cerebral cortex, includes only reticular formations of the brain stem. It is now accepted that the ascending nonspecific activating system takes place from the medulla oblongata to the optic hillock (thalamus).
The reticular (from the Latin word reticulum - mesh) formation consists of numerous groups of neurons that do not have clear boundaries. Such an accumulation of nerve cells by its principle of organization resembles the nerve networks of coelenterates. Their long and highly branching processes form networks around the gray matter of the spinal cord and in the dorsal part of the brainstem. It was first described in the middle of the 19th century, and the name of this structure was given by O. Deiters. In the reticular formation of the brain stem, more than 100 nuclei are isolated, which, from the spinal cord to the diencephalon, are combined into three main groups. 1) The median group of nuclei is concentrated around the midline, mainly in the region of the suture of the bridge and the medulla oblongata (suture nucleus), which are formed by fibers of the sensory pathways extending from the spinal cord, trigeminal nerve nuclei and forming a cross along the midline. 2) The medial group of nuclei is located on the sides of the previous one: it includes the medial large-cell nucleus, bluish place, neurons of the central gray matter of the midbrain, etc. 3) The lateral group of nuclei is located lateral to the medial one and includes the lateral reticular nucleus, parabrachial nuclei, etc.
The neurons of the reticular formation have different sizes: in the median and medial nuclei there are large nerve cells that form long afferent and efferent pathways, and in the lateral ones - medium and small neurons, which are mainly associative neurons.
Most neurons of the reticular formation use peptides (enkephalins, neurotensin, etc.) as a transmitter of nerve impulses, but monoamines are also widely represented. The suture nuclei contain serotonergic neurons, and the bluish nucleus contains noradrenergic neurons.
The connections of the reticular formation are subdivided into afferent and efferent. Afferent fibers end on its neurons: from the spinal cord, following the branches of all sensitive pathways, as well as along the spinoreticular tract, from the nuclei of the cranial nerves as part of the collaterals of the nuclear-cortical, auditory and visual pathways, from the cerebellum as part of the cerebellar-reticular pathway, from the nuclei of the thalamus, subthalamus and hypothalamus, striatum, structures of the limbic system, various parts of the cerebral cortex, including along the branches of the cortical-spinal and cortical-nuclear pathways. The neurons of the reticular formation have long, thin efferent processes, dividing into ascending and descending branches, which are directed to various parts of the brain and spinal cord: motor neurons of the anterior horns of the spinal cord and motor nuclei of the cranial nerves of the brain stem as part of the reticulo-nuclear and reticulo-cerebellar pathways, cerebellum, red nucleus, substantia nigra and nuclei of the roof plate of the spinal cord, reticular nuclei of the thalamus, nuclei of the hypothalamus, indirectly, through the nuclei of the diencephalon to the striatum, limbic system and neocortex.
With the help of the reticular formation, the motor and autonomic nuclei of the brain stem are combined into functional centers that regulate many complex forms of behavior: circulatory, respiratory, cough, swallowing, vomiting, etc. The reticular formation provides: 1) Maintaining a state of wakefulness. By increasing or decreasing the flow of sensory information to the cerebral cortex and subcortical structures, the reticular formation plays the role of a regulator of the level of consciousness (sleep / wake cycle). By regulating the mediator exchange of neurons in the reticular formation or modulating the activity of their receptors with the help of certain drugs, it is possible to activate the activity of the cerebral cortex, or vice versa - to achieve sleep. For example, the caffeine found in coffee or tea stimulates the nerve cells of the reticular formation. On the contrary, among the psychotropic drugs (from the Greek psyche - soul + tropos - direction) there are the so-called neuroleptics, which, by blocking the reticular formation of the brain and reducing the rate of arousal, act in a calming manner (suppress delirium, hallucinations, fear, aggressiveness, psychomotor agitation ). 2) Control of reflex activity by stimulating or inhibiting the motor neurons of the anterior horns of the gray matter of the spinal cord and the motor nuclei of the cranial nerves of the brain stem. 3) Combining a group of neurons from different parts of the brain and spinal cord, which makes it possible to perform complex reflex acts: swallowing, chewing, coughing, vomiting, etc. 4) Providing autonomic regulation due to the coordination of efferent and afferent signals in the corresponding centers of the brain stem. Thus, the vasomotor and respiratory centers unite groups of neurons responsible for the regulation of respiration and blood circulation. 5) Participation in emotional perception of sensitive signals by increasing or decreasing the supply of afferent impulses to the limbic system.
The selective nature of the course of mental processes, which is characteristic of attention, is provided only by the wakeful state of the cortex with an optimal level of excitability. This wakefulness level is achieved due to the work of the mechanisms of communication of the upper trunk with the cerebral cortex and, above all, with the work of the ascending activating reticular formation. It is this ascending activating reticular formation that brings to the cortex, keeping it awake, impulses associated with the body's metabolic processes, drives, with exteroreceptors that bring information from the outside world. First, this flow goes to the upper sections of the trunk and nucleus of the optic hillock, and then to the cerebral cortex.
The provision of optimal tone and wakefulness of the cortex is carried out, however, not only by the ascending activating reticular formation. The apparatus of the descending system is closely connected with it, the fibers of which begin in the cerebral cortex (primarily in the medial and mediobasal regions of the frontal and temporal lobes) and are directed both to the nuclei of the trunk and to the motor nuclei of the spinal cord. The work of the descending reticular formation is very important in that with its help those forms of excitation that initially arise in the cerebral cortex are brought to the nuclei of the brain stem and are the product of higher forms of human conscious activity with its complex cognitive processes and complex programs of life-formed actions.
The interaction of both components of the activating reticular system provides the most complex forms of self-regulation of active states of the brain, changing them under the influence of both elementary (biological) and complex (social in origin) forms of stimulation.
Phylogenetically very ancient neural structure and well-developed part of the reptile brain stem. At first, it was a slow conduction polysynaptic pathway closely associated with the olfactory and limbic regions. The progressive dominance of sight and hearing over the sense of smell led to a shift in sensory and motor functions into the tectum of the midbrain. The straight dorsal and teginal-spinal pathways bypass the reticular formation, which is mainly responsible for autonomic regulation. In mammals, the tectum, in turn, began to play a secondary role in the transmission of excitation along very rapidly conducting fibers connecting the cerebral cortex with peripheral motor and sensory neurons.
In the human brain, the reticular formation retains its connection with the limbic system and continues to play an important role in autonomic and reflex regulation.
Term reticular formation refer only to the polysynaptic neural network of the brainstem, despite the fact that the network extends anteriorly to the thalamus and hypothalamus and posteriorly to the propriospinal tract of the spinal cord.
General structure shown in the figure below. The median reticular formation is formed by a number of suture nuclei (Greek - nuclei raphe). Most of the axial serotonergic pathways nervous system starts from the seam cores.
Reticular formation (RF).(A) Departments. (B) Groups of aminergic and cholinergic cells.
The paramedian reticular formation is located nearby. This section consists entirely of large cell neurons; in the lower part of the pons and the upper part of the medulla oblongata (up to the level of fusion of the reticular formation with the central reticular nucleus of the medulla oblongata), giant cell neurons can also be found.
The most anterior section is considered lateral small cell reticular formation... Long dendrites of small cell neurons branch out at regular intervals. Dendrites have a predominantly transverse direction, and through the gaps between them there are long pathways to the thalamus. The lateral section is formed mainly by afferent neurons. Fibers from all sensitive pathways, including the senses, are suitable for them.
The olfactory fibers pass through the medial forebrain bundle located next to the hypothalamus.
The visual pathways pass through the upper mound.
The auditory fibers come up from the upper core of the olive.
Vestibular fibers approach from the medial vestibular nucleus.
Somatic sensory fibers pass through the spinal reticular tracts from the spinal and own (main or main bridge) nuclei of the trigeminal nerve.
Most of the axons of small-cell neurons are intensively forking between the dendrites of the neurons of the paramedian reticular formation. However, some of them form synapses with the nuclei of the cranial nerves and are involved in the creation of movement programs.
Paramedian reticular formation- predominantly efferent system. The axons are relatively long, with some rising upward, forming synapses with the reticular formation of the brainstem or thalamus. From others, both ascending and descending branches branch off, forming a polysynaptic network. Fibers from the premotor cortex, which give rise to the reticulospinal pathways of the pons and the medulla oblongata, are suitable for large cell neurons.

a) Brainstem aminergic neurons... Groups of aminergic (or monoaminergic) neurons scattered along the reticular formation are neurons whose mediators are formed from aromatic amino acids and have a number of effects on the cell. One group produces the neurotransmitter serotononin, three others produce catecholamines (dopamine, norepinephrine, and adrenaline), and one group produces histamine.
 Serotonergic pathways from the median brainstem (suture).
Serotonergic pathways from the median brainstem (suture).
Serotonergic neurons- the most common neurons in any part of the central nervous system (CNS). These include the neurons of the midbrain, the fibers of which rise to the cerebral hemispheres; pontine neurons branching into the brainstem and cerebellum; cells of the medulla oblongata, descending into the spinal cord.
All parts of the gray matter of the central nervous system are permeated with serotonin-secreting axonal branches. An increase in serotonergic activity is used in clinical practice to treat such a common disease as major depressive disorder.

Dopaminergic neurons of the midbrain are represented by two groups. There is a black substance at the junction of the tire with the legs. Medial to it are the ventral nuclei of the tegmental, from which the mesocortical fibers extend to the frontal lobe and the mesolimbic fibers that go directly to the nucleus accumbens.
Noradrenergic (norepinephrinergic) neurons slightly less abundant than serotonergic. About 90% of neuronal bodies are concentrated in the locus ceruleus in the bottom of the IV ventricle at the upper end of the pons. Paths start from the blue spot in all directions, as shown in the figure below.
 Noradrenergic pathways from the pons and the medulla oblongata.
Noradrenergic pathways from the pons and the medulla oblongata.
Adrenaline-secreting (epinephrine-secreting) neurons relatively few in number and located mainly in the rostral / caudal regions of the medulla oblongata. One part of the fibers ascends to the hypothalamus, the other goes downward, forming synapses with the preganglionic sympathetic neurons of the spinal cord.
In the cerebral hemispheres, the ionic and electrical activity of aminergic neurons is significantly different. First, there are more than one type of postsynaptic receptor for each amine. Second, some aminergic neurons also release protein substances that can regulate the action of the transmitter, usually increasing its duration. Third, the larger cortical neurons receive many excitatory and inhibitory influences from local circulating excitatory networks, and also have many different types of receptors. Activation of one type of aminergic receptor can lead to a strong or weak effect depending on the initial excited state of the neuron.
Our knowledge of the physiology and pharmacodynamics of aminergic neurons is far from complete, but their importance in a wide variety of behavioral functions is beyond doubt.
 Part of a cross section through the upper section of the bridge, showing the elements of the reticular formation.
Part of a cross section through the upper section of the bridge, showing the elements of the reticular formation.
Lecture 3.
RETICULAR FORMATION
Any response of the body, any reflex is a generalized, holistic response to a stimulus. The entire central nervous system is involved in the response, many systems of the body are involved. This union, inclusion in various reflex reactions is provided by the reticular formation (RF). She is the main unifier of the reflex activity of the entire central nervous system.
The first information about the Russian Federation was obtained in the late 19th and early 20th centuries.
These studies have shown that neurons are located in the central part of the brain stem, which have different sizes, shapes and are closely intertwined with each other by their processes. Since the appearance of the nerve tissue in this area under the microscope resembled a network , then Deiters, who first described its structure in 1885, called it the reticular or reticular formation. Deiters believed that the RF performs a purely mechanical function. He considered it as a frame, as a reinforcement of the central nervous system. The true functions of RF, its physiological significance were found out relatively recently, in the last 20-30 years, when the microelectrode technique appeared in the hands of physiologists and using the stereotaxic technique it became possible to study the functions of individual sections of the reticular formation.
The reticular formation is the suprasegmental apparatus of the brain,
Central nervous system. It is associated with many formations of the central nervous system.
The reticular formation (RF) is formed by a set of neurons located in its central parts both diffusely and in the form of nuclei.
Structural features of the RF... RF neurons have long, low-branching dendrites and well-branching axons, which often form a T-shaped branch: one of the branches of the axon has a descending direction, and the other has an ascending direction. Branches of neurons under a microscope form a reticulum (reticulum), which is the reason for the name of this brain structure proposed by O. Deiters (1865).
Classification.
1 ... WITH anatomical point view of the Russian Federation is divided into:
1. The reticular formation of the spinal cord is the substantio Rolandi, which occupies the apex of the posterior horns of the upper cervical segments.
2. Reticular formation of the brain stem (hind and midbrain).
3. Reticular formation of the diencephalon. Here it is represented by nonspecific nuclei of the thalamus and hypothalamus.
4. Reticular formation of the forebrain.
2. Currently, physiologists use the RF classification, which was proposed by the Swedish neurophysiologist Brodal. According to this classification, in the Russian Federation there are lateral and medial fields .
Lateral field- this is the afferent part of the Russian Federation. The neurons of the lateral field perceive information that comes here, enters the ascending and descending pathways. The dendrites of these neurons are directed laterally and they perceive signaling. Axons go towards the medial field, i.e. facing the center of the brain.
Afferent inputs come to the lateral regions of the Russian Federation mainly from three sources:
Temperature and pain receptors along the fibers of the spinoreticular tract and the trigeminal nerve. Impulses go to the reticular nuclei of the medulla oblongata and pons;
Sensory, from the areas of the cerebral cortex along the cortico-reticular pathways go to the nuclei that give rise to the reticulospinal tracts (giant cell nucleus, oral and caudal nuclei of the pons), as well as into the nuclei, which are projected onto the cerebellum (paramedian nucleus and nucleus of the pons lining);
The cerebellar nuclei along the cerebellar-reticular pathway, impulses enter the giant cell and paramedian nuclei and the nucleus of the pons.
Medial field- this is the efferent, executive part of the Russian Federation. It is located in the center of the brain. The dendrites of the neurons in the medial field are directed towards the lateral field, where they contact the axons of the lateral field. The axons of the neurons in the medial field go either up or down, forming the ascending and descending reticular pathways. The reticular pathways, which are formed by the axons of the medial field, form broad connections with all parts of the central nervous system, soldering them together. In the medial field, mainly efferent outputs are formed.
Efferent outputs go:
To the spinal cord along the lateral reticulospinal tract (from the giant cell nucleus) and along the medial reticulospinal tract (from the caudal and oral nuclei of the bridge);
Ascending paths go to the upper parts of the brain (nonspecific nuclei of the thalamus, posterior hypothalamus, striatum), starting in the nuclei of the medulla oblongata (giant cell, lateral and ventral) and in the nuclei of the pons;
Paths to the cerebellum begin in the lateral and paramedian reticular nuclei and in the nucleus of the pons tegmental.
The medial field, in turn, is divided into ascending reticular system (HRV) and descending reticular system (LRS)... The ascending reticular system forms the pathways, directs its impulses to the cerebral cortex and subcortex. The descending reticular system directs its axons in a descending direction - to the spinal cord - the reticulospinal path.
In both the ascending and descending reticular systems, there are inhibitory and activating neurons. For this they distinguish ascending reticular activating system (BPAC), and ascending reticular braking system (ARTS)... VRAS has an activating effect on the cortex and subcortex, while VRTS inhibits and suppresses excitation. LDCs also distinguish descending reticular braking system (NRTS) which originates from the inhibitory neurons of the RF and goes to the spinal cord inhibits its excitation, and descending reticular activating system (HRAS), which sends activating signals in the downstream direction.
Functions of the reticular formation
The reticular formation does not carry out specific, any specific reflexes. The RF function is different.
1. First, the RF provides integration, unification of the functions of the entire central nervous system. It is the main integrating, associative system of the central nervous system. It performs this function because the RF, its neurons form great amount synapses both among themselves and with other parts of the central nervous system. Therefore, when the excitement gets into the RF, it spreads very widely, and radiates along its efferent pathways: ascending and descending, this excitement reaches all parts of the central nervous system. As a result of this irradiation, all formations of the central nervous system are included and involved in the work, and the friendly work of the central nervous system departments is achieved, i.e. RF provides formation of integral reflex reactions, the entire central nervous system is involved in the reflex reaction
II. The second function of the RF is that it maintains the tone of the central nervous system, because RF itself is always in good shape, toned. Its tone is due to a number of reasons.
1). RF has a very high chemotropy Here are neurons that are highly sensitive to certain blood substances (for example, to adrenaline, CO;) and drugs (to barbiturates, chlorpromazine, etc.).
2). The second reason for the RF tone is that impulses from all conductive paths are constantly received in the RF. This is due to the fact that at the level of the brain stem, afferent excitation, which occurs when any receptor is stimulated, is transformed into two currents of excitation. One stream is directed along the classical lemniscal path, along a specific path and reaches a section of the cortex defined for a given stimulation. Simultaneously, each pathway along collaterals deviates into the RF and excites it. Not all pathways act equally on the RF tone. The exciting effect of the conductive pathways is not the same. Particularly strongly stimulates RF impulses, signals that come from pain receptors, from proprioceptors, from auditory and visual receptors. Excitation is especially strong when the endings of the trigeminal nerve are irritated. Therefore, when fainting, the endings n are annoying. trigeminus : doused with water, given to sniff ammonia (yogis, knowing the action of the trigeminal nerve, arrange "brain cleansing" - take a few sips of water through the nose).
3). The RF tone is also maintained by impulses that follow the descending pathways from the cerebral cortex, from the basal ganglia.
4). In maintaining the tone of the mesh formation has great importance also prolonged circulation nerve impulses in the RF itself, the reverberation of impulses in the RF matters. The fact is that in the Russian Federation there is a huge number of neural rings and information, impulses circulate for hours on them.
5). RF neurons have a long latency period of response to peripheral stimulation due to the conduction of excitation to them through numerous synapses.
6). They have tonic activity, at rest 5-10 imp / s.
As a result of the above reasons, the RF is always in good shape and from it impulses are sent to other parts of the central nervous system. If you cut the reticulo-cortical pathways, i.e. the ascending paths going from the RF to the cortex, then the cerebral cortex fails, since it has lost its main source of impulses.
Similar information.
Reticular formation- a set of neurons whose processes form a kind of network within the central nervous system. The reticular formation was discovered by Deiters, studied by V. Bekhterev, and found in the brain stem and spinal cord. The main role is played by the reticular formation of the brainstem. The reticular formation occupies the central part at the level of the medulla oblongata, pons varoli, midbrain and diencephalon. The neurons of the reticular formation are cells of various shapes, they have long branching axons and long non-branching dendrites. Dendrites form synapses on nerve cells. Some dendrites extend beyond the brainstem and reach the lumbar spinal cord - they form the descending reticulospinal pathway.
The reticular formation has connections with various parts of the central nervous system: impulses from various afferent neurons enter the reticular formation. They come along collaterals of other pathways. The reticular formation has no direct contact with the afferent system; the reticular formation has 2-way connections with the neurons of the spinal cord - mainly with motor neurons; with formations of the brain stem (with the diencephalon and midbrain); with the cerebellum, with subcortical nuclei (basal ganglia), with the cerebral cortex.
In the reticular formation of the brainstem, there are 2 departments:
rastral- reticular formation at the diencephalon level;
caudal- reticular formation of the medulla oblongata, pons and midbrain.
48 pairs of nuclei of the reticular formation were studied.
Functions of the reticular formation studied in the 40s. XX century Megun and Morutia. They conducted experiments on cats by placing electrodes in various nuclei of the reticular formation.
The reticular formation has a downward and upward influence.
Downward influence - on the neurons of the spinal cord. It (influence) can be activating and inhibitory.
The upward influence - on the neurons of the cerebral cortex - is also inhibitory and activating. Due to the peculiarities of its neurons, the reticular formation is able to change the functional state of the neurons of the central nervous system.
Features of neurons of the reticular formation:
constant spontaneous electrical activity- provided by the humoral influence and influence of the overlying parts of the central nervous system. This activity has no reflex origin;
convergence phenomenon- impulses go to the reticular formation along the collaterals of various pathways. When converging to the bodies of the same neurons, impulses lose their specificity; impulses, arriving at the neurons of the reticular formation, change its functional activity - if the neurons have a pronounced electrical activity, then under the influence of afferent impulses the electrical activity decreases and vice versa, i.e. the activity of the neurons of the reticular formation is modulated; neurons of the reticular formation have a low threshold of irritation and, as a result, high excitability; neurons of the reticular formation have high sensitivity to the action of humoral factors: biologically active substances, hormones (adrenaline), excess CO2, lack of O2, etc .;
the reticular formation includes neurons with various mediators: adrenergic, choline, serotonin, dopaminergic.
Reticular formation the brain stem is regarded as one of the most important integrative devices of the brain. The integrative functions of the reticular formation proper include:
1) control over the states of sleep and wakefulness,
2) muscle (phase and tonic) control;
3) processing of information signals from the environment and the internal environment of the body, which come through different channels.
The reticular formation unites various parts of the brain stem (the reticular formation of the medulla oblongata, pons varoli and midbrain). Functionally, the reticular formation of different parts of the brain has a lot in common, so it is advisable to consider it as a single structure. The reticular formation is a diffuse accumulation of cells of different types and sizes, which are separated by many fibers. In addition, about 40 nuclei and pidyaders are isolated in the middle of the reticular formation. The neurons of the reticular formation have widely branched dendrites and elongated axons, some of which divide in a T-shaped manner (one process is directed downward, forming the reticular-spinal path, and the second - to the upper parts of the brain).
A large number of afferent pathways from other brain structures converge in the reticular formation: from the cerebral cortex - collaterals of the cortico-spinal (pyramidal) pathways, from the cerebellum and other structures, as well as collateral fibers that approach through the brain stem, fibers sensory systems(visual, auditory, etc.). They all end in synapses on the neurons of the reticular formation. So, thanks to such an organization, the reticular formation is adapted to uniting influences from various brain structures and is able to influence them, that is, to perform integrative functions in the activity of the central nervous system, determining to a large extent the overall level of its activity.
Properties of reticular neurons. The neurons of the reticular formation are capable of sustained background impulse activity. Most of them constantly generate discharges with a frequency of 5-10 Hz. The reason for this constant background activity of reticular neurons is: firstly, the massive convergence of various afferent influences (from receptors of the skin, muscle, visceral, eyes, ears, etc.), as well as influences from the cerebellum, cerebral cortex, vestibular nuclei and others. brain structures on the same reticular neuron. At the same time, excitement often arises in response to this. Secondly, the activity of the reticular neuron can be changed by humoral factors (adrenaline, acetylcholine, CO2 tension in the blood, hypoxia, etc.). These continuous impulses and chemical substances contained in the blood, support the depolarization of the membranes of reticular neurons, their ability to sustained impulse activity. In this regard, the reticular formation also has a constant tonic effect on other brain structures.
A characteristic feature of the reticular formation is also the high sensitivity of its neurons to various physiologically active substances. Due to this, the activity of reticular neurons can be relatively easily blocked by pharmacological drugs that bind to the cytoreceptors of the membranes of these neurons. Especially active in this respect are compounds of barbituric acid (barbiturates), chlorpromazine and others medications, which are widely used in medical practice.
The nature of the nonspecific influences of the reticular formation. The reticular formation of the brain stem is involved in the regulation of the autonomic functions of the body. However, back in 1946, the American neurophysiologist N. W. Megoun and his colleagues discovered that the reticular formation is directly related to the regulation of somatic reflex activity. It has been proven that the reticular formation has a diffuse nonspecific, descending and ascending influence on other brain structures.
Downward influence.
Rising influence. Research N. W. Megoun, G. Moruzzi (1949) showed that irritation of the reticular formation (posterior, midbrain and diencephalon) affects the activity of the higher parts of the brain, in particular the cerebral cortex, providing its transition to an active (non-reliant) state ... This position is confirmed by the data of numerous experimental studies and clinical observations. So, if the animal is in a state of sleep, then direct stimulation of the reticular formation (especially the pons of varoli) through the electrodes inserted into these structures causes a behavioral reaction of awakening of the animal. In this case, a characteristic image appears on the EEG - a change in the alpha rhythm by the beta rhythm, i.e. the reaction of desynchronization or activation is recorded. This reaction is not limited to a certain area of the cerebral cortex, but covers its large arrays, i.e. is generalized. When the reticular formation is destroyed or its ascending connections with the cerebral cortex are turned off, the animal falls into a sonopodifiable state, does not respond to light and olfactory stimuli, and does not actually come into contact with the outside world. That is, the terminal brain ceases to function actively.
Thus, the reticular formation of the brainstem performs the functions of the ascending activating system of the brain, which maintains a high level of excitability of neurons in the cerebral cortex.
In addition to the reticular formation of the brainstem, the ascending activating system of the brain also includes nonspecific nuclei of the thalamus (dim. P. 89), the posterior hypothalamus, and limbic structures. As an important integrative center, the reticular formation, in turn, is part of the more global integration systems of the brain, which include the hypothalamic-limbic and neocortical structures. It is in interaction with them that the appropriate behavior is formed, aimed at adapting the organism to the changing conditions of the external and internal environment.
One of the main manifestations of damage to the reticular structures in humans is loss of consciousness. It happens with craniocerebral trauma, cerebrovascular accident, tumors and infectious processes in the brain stem. The duration of the state of fainting depends on the nature and severity of dysfunctions of the reticular activating system and ranges from a few seconds to many months. Dysfunction of ascending reticular influences is also manifested by loss of vigor, constant pathological drowsiness or frequent bouts of falling asleep (paroxysmal hypersomia), restless night sleep. There are also violations (more often an increase) of muscle tone, various vegetative changes, emotional and mental disorders, etc.
45. Physiology of the cerebellum. The influence of the cerebellum on the motor functions of the body. Symptoms of the cerebellar lesion. Influence of the cerebellum on the autonomic functions of the body.
The cerebellum is a part of the vertebrate brain responsible for coordinating movements, regulating balance and muscle tone.
The cerebellum is a brain center that is extremely important for the coordination and regulation of motor activity and the maintenance of posture. The cerebellum works mainly reflexively, maintaining the balance of the body and its orientation in space. It also plays an important role (especially in mammals) in locomotion (movement in space).
Accordingly, the main functions of the cerebellum are:
1.coordination of movements
2.regulation of balance
3.regulation of muscle tone
4.muscular memory
Symptoms of the defeat.
Disorders of statics and coordination of movements, as well as muscle hypotonia, are characteristic of lesions of the cerebellum. This triad is typical for both humans and other vertebrates. At the same time, the symptoms of cerebellar lesion are described in the most detail for humans, since they have a direct applied value in medicine.
The defeat of the cerebellum, especially its worm (arch- and paleocerebellum), usually leads to disruption of body statics - the ability to maintain a stable position of its center of gravity, providing stability. When this function is disturbed, static ataxia occurs - a movement disorder manifested in a disorder of their coordination. The patient becomes unstable, therefore, in a standing position, he seeks to spread his legs wide apart, to balance with his hands. Static ataxia is especially clearly manifested in the Romberg position. The patient is invited to stand up, tightly moving his feet, slightly raise his head and stretch his arms forward. In the presence of cerebellar disorders, the patient in this position turns out to be unstable, his body sways. The patient may fall. In the case of damage to the cerebellar worm, the patient usually sways from side to side and often falls back, with pathology of the cerebellar hemisphere it tends mainly towards the pathological focus. If the static disorder is moderately expressed, it is easier to identify it in a patient in the so-called complicated or sensitized Romberg pose... In this case, the patient is invited to put his feet on one line so that the toe of one foot rests on the heel of the other. The stability assessment is the same as in the usual Romberg position.
Normally, when a person is standing, the muscles of his legs are tense ( support reaction), with the threat of falling to the side, his leg on this side moves in the same direction, and the other leg comes off the floor ( jump reaction). With damage to the cerebellum, mainly its worm, the patient's support and jump reactions are disturbed. Violation of the support reaction is manifested by the patient's instability in the standing position, especially if his legs are closely shifted at the same time. Violation of the jump reaction leads to the fact that if the doctor, standing behind the patient and insuring him, pushes the patient in one direction or another, then the latter falls with a slight push ( pushing symptom).
The gait of a patient with cerebellar pathology is very characteristic and is called "cerebellar". Due to the instability of the body, the patient walks uncertainly, spreading his legs wide apart, while he is "thrown" from side to side, and if the cerebellar hemisphere is damaged, he deviates from a given direction towards the pathological focus when walking. Instability is especially pronounced when cornering. During walking, the human body is excessively straightened ( Tom's symptom). The gait of a patient with cerebellar lesions is in many ways similar to the gait of a drunk person.
If static ataxia is pronounced, then the patients completely lose the ability to control their bodies and can not only walk and stand, but even sit.
Primary lesion of the cerebellar hemispheres (neocerebellum) leads to a breakdown of its anti-inertial influences and, in particular, to the emergence of dynamic ataxia. It is manifested by the awkwardness of limb movements, which is especially pronounced with movements that require precision. A number of coordination tests are performed to detect dynamic ataxia.
Test for diadochokinesis - the patient is invited to close his eyes, stretch his arms forward and quickly, rhythmically supinate and pronate (rotate outward and inward) the hands. In case of damage to the cerebellar hemisphere, the movements of the hand on the side of the pathological process turn out to be more sweeping, as a result, this hand begins to lag behind. Then they talk about the presence of adiadochokinesis.
Finger-nose test - a patient with closed eyes removes his hand, and then with his index finger tries to get into the tip of his nose. In the case of cerebellar pathology, the hand on the side of the pathological focus makes an excessive movement in volume, as a result of which the patient misses. Also, an intentional tremor (tremor of the fingers), characteristic of cerebellar pathology, is revealed, the severity of which increases as the finger approaches the target.
Heel-knee test - a patient lying on his back with his eyes closed, raises his leg high and tries to hit the knee of the other leg with his heel. With cerebellar pathology, a miss is noted, especially when performing a homolateral test (on the same side) to the affected cerebellar hemisphere with the leg. If, nevertheless, the heel reaches the knee, then it is proposed to hold it, slightly touching the lower leg, along the crest of the tibia down to the ankle joint. Moreover, in the case of cerebellar pathology, the heel slides all the time in one direction or the other.
Index (finger-toe) test - the patient is invited to get his index finger into the tip of the investigator's finger directed at him. In the case of cerebellar pathology, a mimic fall is noted. In this case, the patient's finger usually deviates towards the affected cerebellar hemisphere.
Symptom Tom-Jumenti - grabbing an object, the patient spreads his fingers disproportionately wide.
"Test with a bowl" - a patient, holding a glass of water in his hand, splashes water.
Nystagmus - twitching of the eyeballs when looking to the sides or up. When the cerebellum is affected, nystagmus is considered as the result of intentional tremor of the eyeballs. In this case, the plane of nystagmus coincides with the plane of arbitrary eye movements - when looking to the sides, nystagmus is horizontal, when looking up - vertical.
Speech disorder - occurs as a result of a violation of the coordination of the muscles that make up the speech motor apparatus. Speech is made slower (bradilalia), its smoothness is lost. She gets explosive chanted character (accents are placed not according to meaning, but at regular intervals).
Changes in handwriting - the patient's handwriting becomes uneven, the letters are distorted, excessively large ( megalography).
Stuart-Holmes symptom (a symptom of the absence of a reverse push) - the researcher asks the patient to bend the supinated forearm and at the same time, taking his hand by the wrist, resists this movement. If the examiner unexpectedly releases the patient's hand, the patient will not be able to slow down further flexion of the arm in time, and it, bending by inertia, will forcefully hit him in the chest.
Pronatory phenomenon - the patient is asked to hold his arms outstretched forward, palms up. In this case, spontaneous pronation occurs on the side of the affected cerebellar hemisphere (turning the palm inward and downward).
Hoffa-Schilder's symptom - if the patient holds his arms outstretched forward, then on the side of the pathological focus the hand is pulled outwards.
Doinikov's phenomenon (change in postural reflexes) - a seated patient is invited to put his hands with fingers apart on his hips, palms up, and close his eyes. In the case of cerebellar pathology, spontaneous flexion of the fingers and pronation of the hand are noted on the side of the pathological focus.
Schilder's test - the patient is offered to stretch his arms forward, close his eyes, raise one hand up and lower it to the level of the other hand, and then do the opposite. If the cerebellum is damaged, the patient will lower his arm below the outstretched one.
Muscle hypotension is detected during passive movements made by the examiner in various joints of the patient's extremities. The defeat of the cerebellar vermis usually leads to diffuse muscle hypotonia, while with damage to the cerebellar hemisphere, a decrease in muscle tone is noted on the side of the pathological focus.
Pendulum reflexes are also caused by hypotension. In the study of the knee reflex in a sitting position with legs freely hanging from the couch after a blow with a hammer, several "rocking" movements of the lower leg are observed.
Asynergy- loss of physiological synergistic (friendly) movements during complex motor acts.
The following tests for asynergy are most common:
A patient standing with shifted legs is asked to bend back. Normally, simultaneously with throwing back the head, the legs synergistically bend at the knee joints, which allows maintaining the stability of the body. With cerebellar pathology, there is no friendly movement in the knee joints and, throwing his head back, the patient immediately loses his balance and falls in the same direction.
The patient, standing with shifted legs, is invited to lean on the palms of the doctor, who then unexpectedly removes them. If the patient has cerebellar asynergy, he falls forward ( Ozhekhovsky symptom). Normally, there is a slight deviation of the body back, or the person remains motionless.
A patient lying on his back on a firm bed without a pillow, with his legs spread apart to the width of the shoulder girdle, is asked to cross his arms over his chest and then sit down. Due to the absence of friendly contractions of the gluteal muscles, a patient with cerebellar pathology cannot fix the legs and pelvis to the support area, as a result, he cannot sit down, while the patient's legs, coming off the bed, rise up (asynergy according to Babinsky).
Influence of the cerebellum on autonomic functions. The cerebellum has a depressing and stimulating effect on the work of the cardiovascular, respiratory, digestive and other body systems. As a result of the dual influence, the cerebellum stabilizes and optimizes the functions of the body's systems.
The cardiovascular system reacts to irritation of the cerebellum either by increasing (for example, pressor reflexes) or by decreasing this reaction. The direction of the reaction depends on the background on which it is triggered. When the cerebellum is irritated, high blood pressure decreases, and an initial low blood pressure rises. Irritation of the cerebellum against the background of rapid breathing (hyperpnea) reduces the respiratory rate. In this case, unilateral irritation of the cerebellum causes a decrease on its side, and on the opposite side - an increase in the tone of the respiratory muscles.
Removal or damage to the cerebellum leads to a decrease in the tone of the intestinal musculature, due to the low tone, the evacuation of the contents of the stomach and intestines is disturbed. The normal dynamics of secretion and absorption in the stomach and intestines is also impaired.
Metabolic processes with damage to the cerebellum are more intense, the hyperglycemic reaction (an increase in the amount of glucose in the blood) to the introduction of glucose into the blood or to taking it with food increases and lasts longer than normal, appetite worsens, emaciation is observed, wound healing slows down, skeletal fibers muscles undergo fatty degeneration.
When the cerebellum is damaged, the generative function is disrupted, which manifests itself in a violation of the sequence of the processes of labor. When the cerebellum is excited or damaged, muscle contractions, vascular tone, metabolism, etc., react in the same way as when the sympathetic division of the autonomic nervous system is activated or damaged.
Thus, the cerebellum takes part in various types of body activity: motor, somatic, autonomic, sensory, integrative, etc. However, the cerebellum realizes these functions through other structures of the central nervous system. The cerebellum performs the function of optimizing the relationship between different parts of the nervous system, which is realized, on the one hand, by activating individual centers, on the other, by keeping this activity within certain limits of excitation, lability, etc. After partial damage to the cerebellum, all functions of the body can be preserved, but the functions themselves, the order of their implementation, the quantitative correspondence to the needs of the organism's trophism are violated.
Thus, the cerebellum plays a primary role in the regulation of posture and movement. Many movements can only be optimally performed with the participation of the cerebellum. At the same time, it does not belong to the number of vital organs, since people born without a cerebellum do not have serious movement disorders. The cerebellum has two hemispheres and has a gray matter cortex. The cortex contains cells with numerous dendrites that receive impulses from many sources associated with muscle activity: proprioceptors of tendons, joints and muscles, as well as from the motor centers of the cortex. Therefore, the cerebellum integrates information and coordinates the work of all muscles involved in movement or posture maintenance. If the cerebellum is damaged, the movements become sharp, not smooth. The cerebellum is absolutely essential for coordinating fast movements such as running, typing on a keyboard, and speaking.
All functions of the cerebellum are carried out without the participation of the cerebral cortex, i.e. unconsciously. However, in the early stages of ontogeny or learning, they may include training elements. At this time, the cortex controls the cerebellum, and certain volitional efforts are required to implement motor acts. For example, this is the case when learning to ride a bicycle, swimming, etc. After the development and consolidation of motor acts, the cerebellum takes over the function of controlling the corresponding reflexes.
43. Descending influences of the reticular formation. Its participation in the regulation of muscle tone.
Downward influences. In R. f. distinguish between areas that have inhibitory and facilitating effects on motor reactions spinal cord.
When the reticular formation of the hindbrain is irritated (especially the giant cell nucleus of the medulla oblongata and the reticular nucleus of the pons, where the lobule of the reticulospinal pathway is taken), all spinal motor centers (flexion and extensor) are inhibited. This inhibition is very deep and prolonged. This situation in natural conditions can be observed during deep sleep.
Along with diffuse inhibitory effects, when certain areas of the reticular formation are irritated, diffuse
influence that facilitates the activity of the spinal motor system.
The reticular formation plays an important role in the regulation of the activity of muscle spindles, changing the frequency of discharges delivered by gamma-efferent fibers to the muscles. This modulates the reverse impulse in them.